Abstract
Background:
Minimal residual disease (MRD) quantification prior to allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a powerful predictor for post-transplant outcome. Thus, new strategies with modified transplantation procedures are needed to reverse the outcomes of that remain MRD-positive despite multiple induction attempts.
OBJECTIVE:
To determine the prognostic relevance of MRD status in patients with acute lymphoblastic leukemia (ALL), especially those with Philadelphia chromosome-positive ALL (Ph+ ALL), receiving the conditioning regimen of FA5-Bucy, registered on http:// ClinicalTrials.gov (NCT02328950).
METHODS:
We retrospectively reviewed our HSCT experience using FA5-Bucy, i.e., 5-day salvage chemotherapy (Fludarabine/Ara-C) and conditioning (Busulfan/ Cyclophosphamide) for patients with ALL. A total of 48 consecutive patients from 2013 to 2016 are analyzed. 11 out of 48 (7 males and 4 females) were diagnosed with Ph+ ALL with the induction treatments including a tyrosine kinase inhibitor (TKI). Median age was 30 years (range, 8-52 years). Among whom four (36.4%) achieved complete remission(CR)at transplantation, Six (54.5%) with detectable residual P190 BCR-ABL positive leukaemic cells, while 1 (9.1%) not in the status of remission with 39.5% blasts in the bone marrow (BM). The other 37 cases were Ph-negative (Ph-) ALL, with the median age of 21 years (range, 2-61 years). Among whom 25 (67.6%) patients were in CR, 6 (16.2%) MRD-positive and 6 (16.2%) with 23.5%-98% BM blasts. The MRD status was monitored by four-color FCM in Ph- group, and by RT-PCR to detect the chimeric bcr-abl mRNA transcript in Ph+ group. Patients were transplanted either from an HLA-identical sibling or haplo-identical related donors. The GVHD prophylaxis consisted of ATG, CsA, MMF and short-term MTX. None of these patients had severe infection or organ failure before HSCT.
RESULTS:
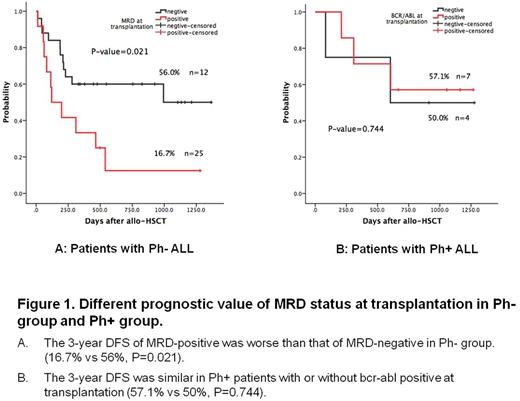
All patients achieved successful engraftment and full donor chimerism. Patients with Ph+ ALL seems have a better outcome than that with Ph- ALL (3-year OS of 54.5% vs 37.8%, P=0.245). With a median follow-up of 666 (83-1276) days, the 1y-OS and 1y-DFS were 72.7%, 3y-OS and 3y-DFS were 54.5% in Ph+ group, respectively, and non-relapse mortality and relapse incidence were 18.2% and 10%. MRD monitoring is an important tool for relapse prediction in Ph- ALL patients (3-year OS and DFS of MRD-positive vs MRD-negative =16.7% vs 56%, P=0.021).However, the profile of OS and DFS was similar in Ph+ patients with bcr-abl positive to that with bcr-abl negative (3-year OS and DFS of bcr-abl positive vs bcr-abl negative= 57.1% vs 50%, P=0.744). Severe acute-GvHD (aGVHD) occurred in 3/11 patients. Few patients experienced mild-to-moderate toxicity, and main causes of death were aGVHD.
CONCLUSION:
We concluded that allo-HSCT with the sequential tumor-ablative conditioning of FA5-Bucy offers great benefits for the patients with Ph+ ALL, with the potentially capability of reducing or overcoming the negative impacts of MRD. Thus creates exciting transplant opportunities for patients not in remission to be cured.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal